By: Jeffrey Yaskin, PT, MPT, MTC, CSCS
Do you know how to squat? Squatting is an activity that we should be performing many times throughout the day, hopefully, without even thinking about it nor realizing we are doing it. We don’t think much about walking from one spot to another and nor should we think much about squatting from a standing position down to the ground. Squatting is very healthy for the musculoskeletal system and as well as for the gastrointestinal system. It is also a very functional movement. Somewhere along the line, unfortunately, some people have come to the conclusion that squatting is bad for you. In this first of a 3 part series on squatting, we will touch on the functional aspects of squatting.
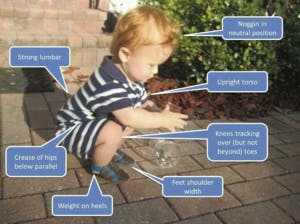
A child naturally squats to interact with objects on the floor. If you have children aged 1 to 5 and they are playing with items on the floor they simply squat down and “sit” in the squatting position with no issue until they are ready to stand. What you do not see is a child that age bending over to reach the same object on the floor. “The squat position is typically acquired after 10-12 months of development”(1). Squatting is more stable than standing which is why children adopt it earlier than standing. “ Standing in free space is not typically achieved until a child reaches 12-14 months of development”(2). Why squat over bend? Squatting is more stable and places less stress on your joints. Bending over in a standing position is less stable and places much more stress on your lower back. Interestingly, at this young age no one tells nor teaches the young child to perform this activity, it is innate. We all squatted this way and it begs us to question, why did we stop as we became older.

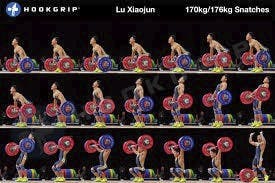
Were you glued to the TV watching the Olympics this summer? I believe it was during the wee hours of the night that the Olympic Lifting portion was telecast. With the explosion of Crossfit as an exercise philosophy, Olympic Lifting has become mainstream. The two lifts are the clean and jerk and the snatch. Both start in a deep squat position with the bar on the ground. Lift the bar with an upright trunk to the chest and stabilize yourself in another deep squat with the bar resting on your shoulders. In the clean and jerk, the second squat you have the bar resting on your shoulders and then you stand up pressing the bar overhead. “The clean tells you a lot about an athlete”(3). In the snatch, the second squat you have landed with the bar pressed overhead and then you stand up with the bar pressed overhead. “Nothing will tell you more about an athlete’s range of motion and understanding of the midline stabilization and torque principles than the snatch”(4). Both lifts are extremely technical and require copious amounts of time training to fully master. Any Olympic Lifting coach worth their mettle will agree that both of these lifts begin and end with a perfect squat.

If you have ever been to a train station in one of the older and smaller Italian towns and have to use the restroom you were probably met with a hole in the ground. What am I supposed to do with that? Squat! That’s right squat down and do your business. Prior to the invention of the toilet we defecated as humans by deep squatting. “Squatting has been the natural defecation position for humans since time immemorial “(6). If you have ever been exercising outside and had to move your bowels you simply squatted down and no problem. “There is a muscle that encircles the gut like a lasso when we are sitting or standing, and it pulls the gut in one direction, creating a kink in the tube “(7). “Squatting leads to a nice straight intestinal tract, allowing for a direct, easy exit “(8). I know many of us are dog owners and how does your dog poop? Sitting? No they squat down! “Hemorrhoids, digestive diseases like diverticulitis and even constipation are common only in countries where people generally sit on some kind of chair to pass their stool.”(9) So for the health of your bowels add more squatting to your daily routine.

Properly functioning pelvic floor muscles are synonymous with deep squatting and are necessary for pelvic stability and proper bowel and bladder health. “Once below a parallel squat, a quad dominant individual will not be able to maintain balance. This person will fall backward, unable to release tension in the quadriceps to allow the glutes, pelvic floor and core musculature to take over and stabilize” (10). A stable squat involves proper balance of the quads, glutes, pelvic floor and core muscles. The pelvic floor muscles become eccentrically lengthened during a deep squat. Squatting increases the size of the pelvic outlet by 1-2 cm vs standing position. “By forcing the upper leg bones (femur) to act like levers on your pelvic bones, you can widen your pelvis opening by 20-30 percent” (11). Squatting with knees pushed out wide increases tension in the hip adductor muscles pulling on the pubic bones and opening the pelvic canal. The levator Ani muscles (pelvic floor muscles) counter the pull from the adductor muscles. This helps keep them healthy and functioning properly. Properly squatting deep throughout the day helps to keep the pelvic floor muscles functional.
One way to assess your squat and muscle balance is Durango is a through a Functional Movement Screen(FMS). This is a seven-part screen for people without pain who want their basic movement ability profiled. This movement screen was created in 1998 and currently is standard practice in assessing Special Forces Operators, NFL-NBA-NHL-MLB players and Olympic athletes. Guess what movement is the first tested in the FMS? The Overhead Squat. Watching a person squat with their arms in an overhead position is very telling about that person’s movement health and efficiency. “Extremity mobility, postural control, pelvic and core stability are well represented in the deep squat movement pattern. The deep squat is a move that challenges total body mechanics and neuromuscular control when performed properly” (5). Are you starting to understand how important the simple squat is in our daily lives? We are certified in assessing the FMS and would be happy to screen you as part of our free injury screen program.

Thus far we have discussed many reasons to squat daily. Its functional and it helps to maintain the health of the viscera, hips,and pelvic floor musculature. In the second and third parts of this squat analysis we will closely look at what is considered a proper way to squat and the many faults related to squatting poorly.
References:
(1), (2): Kobesova, A, Safarove, M. and Kolar, P. Dynamic neuromuscular stabilization: Exercise in the developmental positions to achieve spinal stability and functional joint centration. In: Hutson, M. and Ward, A (Eds.), Oxford Textbook of Musculoskeletal Medicine. Oxford University Press: 66-83, 2015.
(3), (4): Starrett, Dr. K. Becoming a Supple Leopard: The ultimate guide to resolving pain, preventing injury, and optimizing athletic performance. Victory Belt Publishing: 183, 195, 2013.
(5), (10): Cook, G. Movement: Functional movement Systems. On Target Publications: 90, 196, 2010.
(6), (7), (8), (9): Enders, G. Gut: The Inside Story of Our Body’s Most Underrated Organ. Greystone books: 17, 18, 2015.
(11): Russell, J.G.B., “Moulding of the Pelvic Outlet”,J. Obstet. Gynaec. Brit. Cwlth, Sept. 1969, Vol. 76, pp. 817-820.







 <?div>
<?div>



